Abstract
Introduction. No data are available in literature about the relationship between gender and the development of CMR abnormalities and/or cardiac complications in sickle cell disease (SCD). This prospective and multicentre study aimed to assess if there was an association between gender and risk of cardiac iron overload, heart dilation, hypertrophy, and dysfunction, and myocardial fibrosis, assessed by Cardiovascular Magnetic Resonance (CMR), and of cardio-vascular complications in sickle cell disease (SCD) patients.
Methods. We considered 115 SCD patients (58 females, 34.79±13.26 years), consecutively enrolled in the Myocardial Iron Overload in Thalassemia (MIOT) Network. Myocardial iron overload was assessed by the multislice multiecho T2* technique. Biventricular function parameters and atrial areas were quantified by cine images. Late gadolinium enhancement (LGE) images were acquired to detect myocardial fibrosis.
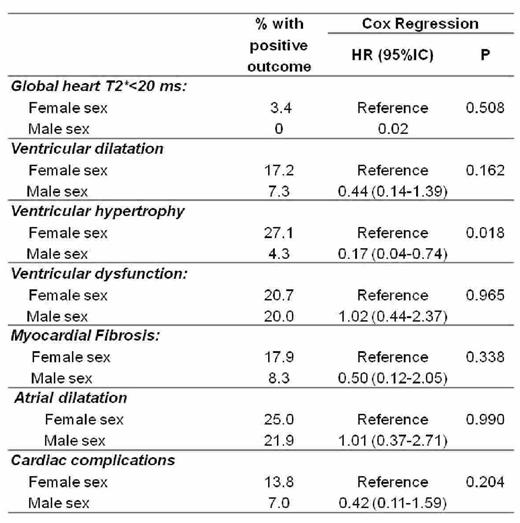
Results. Table 1 shows the comparison between sexes in the development of cardiac outcomes.
Males and fameles showed a similar risk of accumulating cardiac iron, but both patients with cardiac iron were females.
Compared to females, males showed a significant lower risk of developing biventricular hypertrophy (Kaplan-Meyer curve shown in Figure 1), although having a similar risk for biventricular dilation and dysfunction and for myocardial fibrosis. No patients with less than 34 years developed biventricular hypertrophy and age at the CMR was significantly higher in patients with hypertrophy versus patients without it (42.93±7.23 years versus 34.64±12.79 years; P=0.001).
We recorded 12 (10.4%) cardiac events: 4 ischemic strokes, 5 arrhythmias (4 supraventricular and 1 ventricular), two pulmonary hypertensions and one pulmonary embolism. No prospective association was detected between gender and cardiac complications.
Conclusion. In SCD male and female seem to show a comparable risk in developing cardiac complication, although compared to females, males showed a significant lower risk of developing biventricular hypertrophy. There are no specific guidelines for SCD patients and, as a consequence, the cardiovascular follow-up is conformed to that one of thalassemia patients (complete cardiac evaluation performed annually for both genders). Our data not support a different follow up time based on the gender.
Pepe: Chiesi Farmaceutici and ApoPharma Inc.: Other: Alessia Pepe is the PI of the MIOT project, that receives no profit support from Chiesi Farmaceutici S.p.A. and ApoPharma Inc.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal